Medical Benefits
Welcome
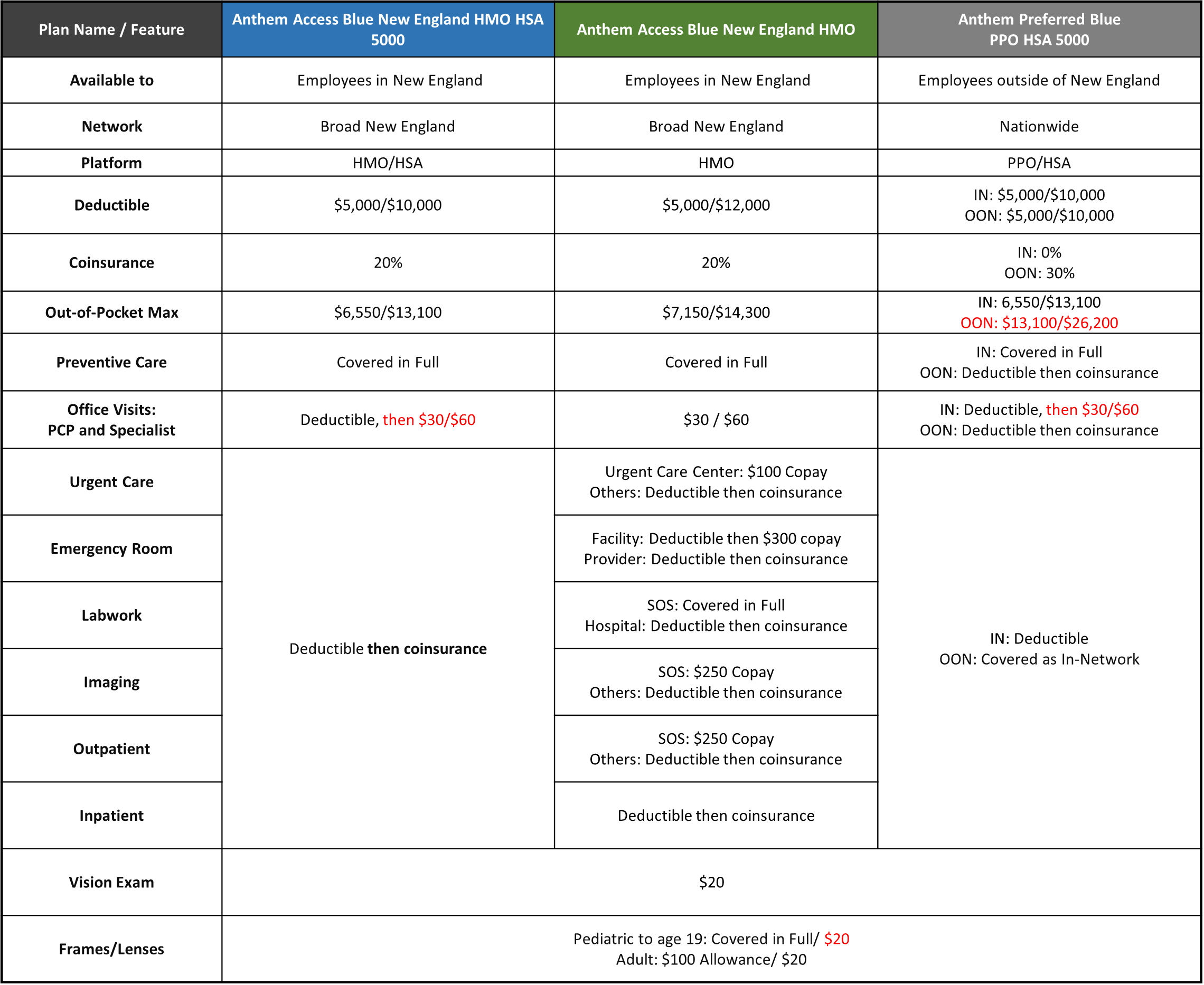
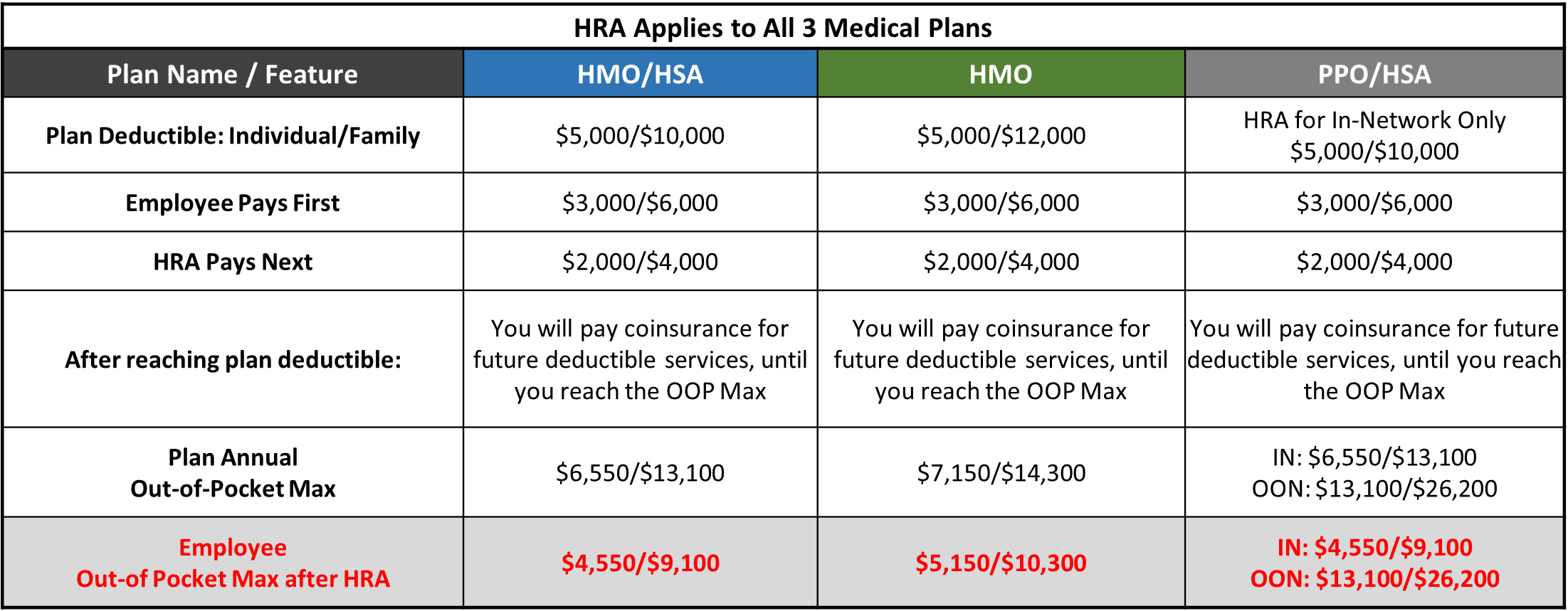
Powers offers two high-deductible HSA-eligible health insurance plans through Anthem. The Access Blue New England HMO HSA 5000 is for employees living in New England. The Preferred Blue PPO HSA is for employees living outside of New England. Powers also offers a third plan option; the Access Blue New England HMO SOS 5000. Plan features are summarized below for your convenience. If there are discrepancies between information on this page and Anthem produced documents, please rely on the latter.
Eligibility
All regular full-time employees working 30+ hours a week are eligible to enroll in health insurance. Eligibility for newly hired employees is first of the month, following 30 days of full-time employment.
Benefit Information
How do I enroll?
Open Enrollment is your time to make new benefit elections or make changes to your current benefit elections. During Open Enrollment, Oct 27th- November 10th 2023, your health insurance enrollment form must be completed and returned to Human Resources.
Newly hired, regular full-time employees will enroll for health insurance benefits during the new employee orientation period. Eligibility begins on the first of the month, following the 30 days of employment.
Waiving or Declining Health Insurance
If you are eligible for health insurance and will not be enrolling because of alternative coverage, or choose not to have insurance, a waiver form must be signed during the enrollment period. If you elect not to enroll, you may not join the plan until the next Open Enrollment period, unless there is a “qualifying event.” A Qualifying Life Event is a life-changing situation that allows you to make changes to your benefit elections, outside of the normal, Open Enrollment period. Examples of Qualifying Life Events include: the birth of a child, marriage, divorce and a loss of other coverage.
All employees should be aware of possible Federal tax penalties for declining Powers’ health insurance plan enrollment, as well as alternatives for health insurance available through the Health Insurance Exchange. For more information about declining health insurance, see: https://www.healthcare.gov/getcoverage/ and http://www.valuepenguin.com/ppaca/exchanges/nh.
What happens if I leave Powers?
Under certain circumstances, you and your dependents may continue to participate in health coverage, dental insurance, and the Medical Flexible Spending Account through the Consolidated Omnibus Budget Reconciliation Act (COBRA). COBRA is a federal guarantee of the continuation of health insurance plan coverage after employment ends, which allows you to remain on medical and dental coverage, at the employee’s expense, for up to 18 or 36 months, depending on the circumstances. Former employees who enroll via COBRA will be responsible for the full cost of the monthly premiums.
Summary of Benefits & Coverages
Powers offers two high-deductible HSA-eligible health insurance plans through Anthem. The Access Blue New England HMO HSA 5000 is for employees living in New England. The Preferred Blue PPO HSA 5000 is for employees living outside of New England. Powers offers a third plan option; the Access Blue New England HMO SOS 5000.
There are three major components of a Health plan.
Network – The Access Blue New England plans offer a Broad New England Network while the Anthem Preferred Blue PPO HSA 5000 offers a nationwide network outside of New England.
Cost To Use – You will be responsible for meeting the deductible before paying a copay, for most services under the Anthem Access Blue New England HMO HSA 5000 plan. The deductibles for this plan are $5,000 (single) and $10,000 (family). The Out-of-Pocket Maximums are $6,550 (single) and $13,100 (family). The Anthem Access Blue New England HMO plan has deductibles of $5,000 (single) and $12,000 (family) and Out-of-Pocket Maximums of $7,150 (single) and $14,300 (family.) The third plan that Powers offers is the Anthem Preferred Blue PPO HSA 5000 which has deductibles of $5,000 (single) and $10,000 ( family). The deductibles are the same for in-network and out-of-network coverage. The Out-of-Pocket Maximums are $6,550 (Single) and $13,100 (family) for In-Network coverage and $13,100 (single) and $26,200 (family) for Out-of-Network Coverage. $20% Coinsurance will be paid after meeting the deductible under the Anthem Access Blue New England HMO HSA 5000 and the new Anthem Access Blue New England HMO for Inpatient and Outpatient services, until the Out-of-Pocket Maximum (OOP) has been met. The Out-of-Pocket maximum refers to the most you will pay for covered expenses under each plan. The Anthem Preferred Blue PPO HSA 5000 has no coinsurance for In-Network and 30% co-insurance for Out-of-network.
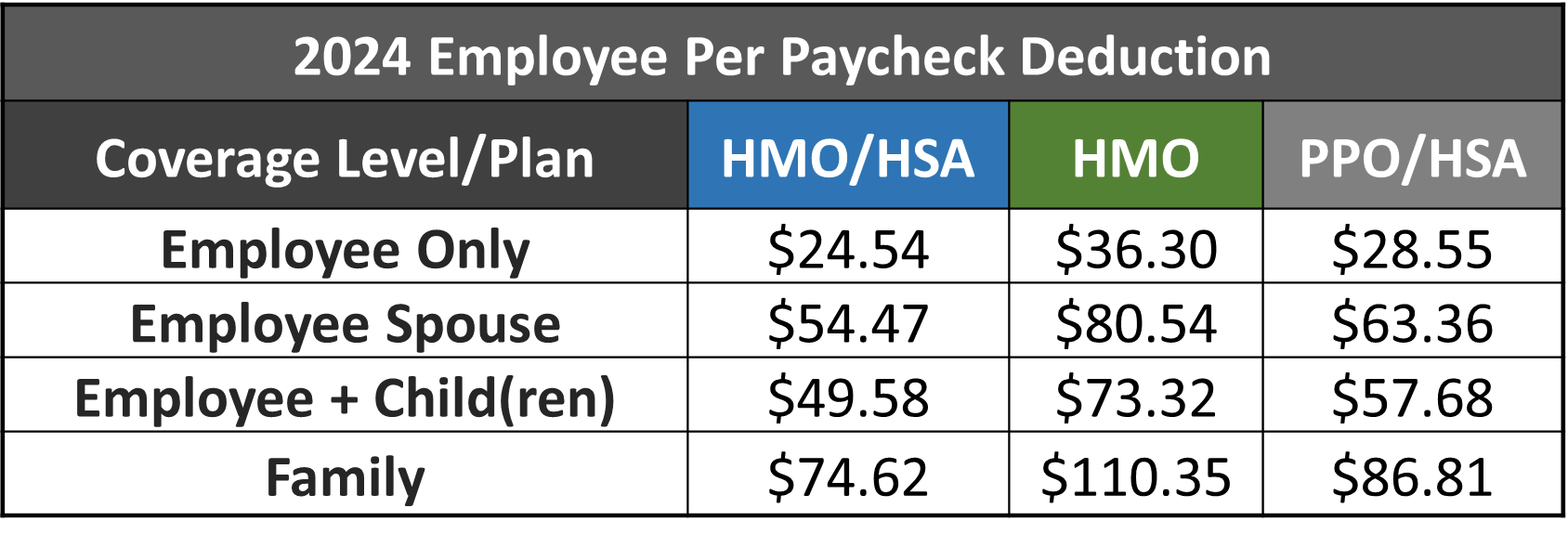
Cost To Own – Powers pays for 75% of the cost of employee Health insurance. Employees pay 100% of the cost to cover their spouse and/or children. The amount that will be deducted from each paycheck is listed below.
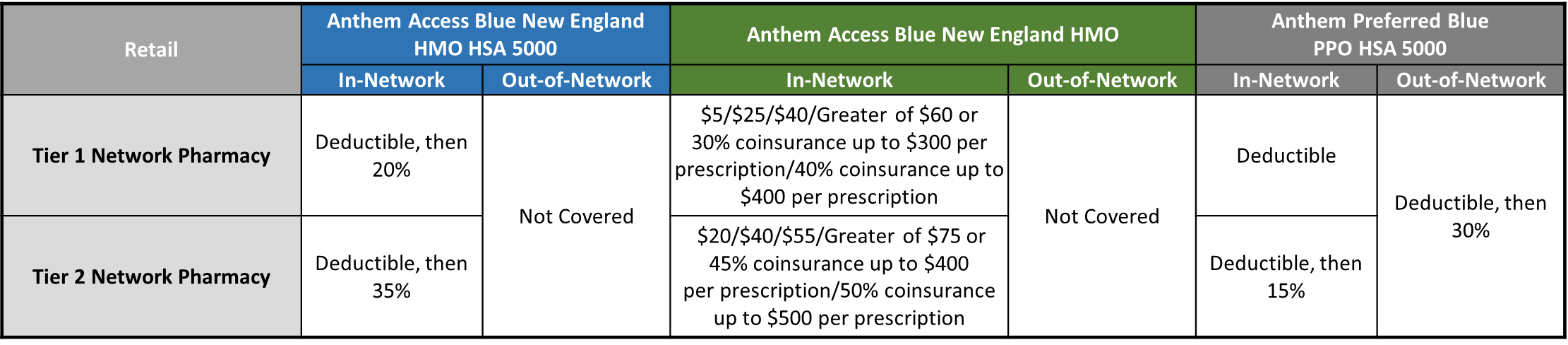
Powers offers three health insurance plans through Anthem. The Access Blue New England HMO HSA 5000, the Access Blue New England HMO SOS 5000 and the Preferred Blue PPO HSA. All three of Powers’ medical plans offer prescription drug benefits that operate on the Rx Choice Tiered Network.
The following link will bring you to Powers’ Anthem Rx Formulary.
https://www.anthem.com/ms/pharmacyinformation/home.html
After the above link, click on “Essential Drug List 4-Tier” and enter your RX name.
Contributions & Rates
The chart below shows the weekly payroll deduction for various coverage levels of each plan.
Carrier Contact Information
Plan Documents
Additional Information
Health Reimbursement Arrangement
Health Reimbursement Arrangement (HRA)
What is a Health Reimbursement Arrangement (HRA)?
An HRA is an account used to reimburse employees for deductible-eligible expenses. The employee may submit for reimbursement after a qualifying expense has been incurred.
Who is eligible?
Enrollment in the HRA is automatic when you enroll in one of Powers’ Anthem Health Insurance Plans.
HRA Allowance
Powers funds a Health Reimbursement Account (HRA) to reimburse employees for deductible-eligible expenses associated with their Powers Anthem health insurance. Employees are responsible for the first $3,000 (single) or $6,000 (Family) of deductible expenses for themselves and/or their dependents. After having paid $3,000 or $6,000 in eligible expenses, you are able to submit for reimbursement for any additional, eligible expenses incurred up to the total deductible. You can use the money in the HRA throughout the year for qualified deductible medical expenses. And, because the money contributed by Powers doesn’t count as income, there are no tax implications for you.
Who pays the provider?
You. After you’ve received the provider invoice, and the Explanation of Benefits (EOB) from Anthem, you should review the information to confirm the claim was processed correctly, then pay the provider the amount the EOB says you owe.
How do I get reimbursed?
American Benefits Group administers Powers’ HRA. Once you incur $3,000 ($6000 if you have dependents) of deductible-eligible services, processed by Anthem and reflected on your Anthem Explanation of Benefits (EOB) you may submit a request for reimbursement from the HRA to ABG, one of three ways:
Online
- www.amben.com/wealthcare
- Employer ID: ABGPGS
- Your Social Security Number
- Complete distribution request form and submit Anthem Explanation of Benefits
- Claims@amben.com
- Attach completed HRA Reimbursement form (see HR or www.amben.com)
- Attach Anthem Explanation of Benefits
Fax
- Fax Reimbursement Request Form & Anthem EOB to 877-723-0147
For Reimbursement amounts and limits, please see the chart below.
What if I don’t use the full benefit by the end of the plan year?
You will have 90 days (through 3/31) to request reimbursement for deductible-eligible expenses incurred during the previous plan year. After 4/1, any unused amounts will be forfeited.
Carrier Contact Information

AMerican Benefits Group: (HRA) Health Reimbursement Arrangement
Customer Service: 800-499-3539
Website: www.amben.com
Company ID: ABGPGS
Forms and Plan Documents
Health Savings Account
Health Savings Account (HSA)
What is a Health Savings Account (HSA)?
An HSA is a triple-tax-advantaged trust/custodial account that eligible individuals can use to pay for qualified medical, dental & vision expenses for themselves or their tax dependents.
Who is eligible?
Enrollment in the HSA is automatic when you enroll in one of Powers’ Anthem Health Insurance Plans.
Triple-tax-advantaged: Contributions are pretax, contributions accumulate tax-free, distributions for qualified expenses are tax-free.
Contributions may be made either through payroll deduction or directly to Health Equity from your personal account.
Contribution limits in 2024, are $4,150 for single coverage; $8,300 for dual/family coverage. If age 55+ additional $1000.
You may pay for eligible expenses with the debit card issued by Health Equity, or using another form of payment and requesting reimbursement from your HSA.
Funds in your HSA account will accumulate and grow until you remove them. If your employment ends at Powers your account can remain with Health Equity. If you enroll in another HSA-eligible health insurance plan, and remain eligible to make contributions, you may resume contributions. If you are not enrolled in an HSA-eligible health insurance plan you may use the funds to pay for qualifying medical expenses but will be unable to make future contributions.
While your HSA account belongs to you, and you may use the funds for any purpose, withdrawals/distributions for purposes other than qualifying medical expenses while be taxed as ordinary income and subject to a 20% penalty tax before age 65. After age 65, 20% penalty not assessed, but distributions for expenses other than qualified medical will be taxed.
For convenience, Powers has established a relationship with HSA custodian Health Equity. www.healthequity.com.
Carrier Contact Information

Health Equity: (HSA) Health Savings Account
Customer Service: 866-346-5800
Website: www.healthequity.com
Forms and Plan Documents
HSA Store
The Richards Group has entered into a partnership with Health-E Commerce, also known as the HSA Store. This gives you access to hundreds of products that have been pre-vetted & approved for use with your Health Spending Account.
Did you know you could use your HSA to save money on everyday health essentials like baby health items, health trackers, pain relief products and more?
Here are just a few benefits of using the HSA Store:
- No Receipts Needed
- 2,500+ FSA Eligible Products
- 100% Eligibility Guaranteed
- Skip the claims process when you use your HSA card

This partnership also allows access to their Caring Mill products. Caring Mill is a line of premium healthcare products that support a healthy lifestyle and on average is priced 30% less than branded equivalent products.

With every Caring Mill purchase, a donation is made to Children’s Health Fund, providing necessary treatments to thousands of children in need, throughout the United States.
Curious what your HSA dollars can cover? Simply enter the product you are looking for in the eligibility list below.
Dental Benefits
Eligiblity
All full-time employees who work a minimum of 30 hours per week are eligible, first of the month following 30 days of employment.
Summary of Benefits and Coverages
Plan Overview
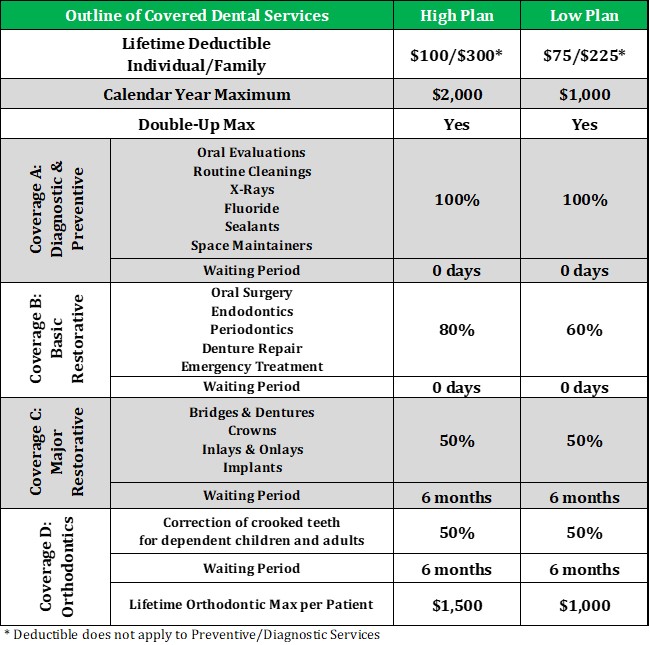
Powers offers it’s employees the Basic Plus and Premium Plus plans through Northeast Delta Dental. The plans covers Preventive Care, Minor and Major Restorative procedures, as well as Orthodontia.
The chart below provides a high level overview of the dental plan design and features offered to eligible employees by Powers Guaranteed.
When considering whether purchasing dental insurance makes sense for you and your family, there are three things you should consider:
Network – Northeast delta dental has an extensive network. For a complete list of in-network dentists, visit https://portal1.nedelta.com/DentistSearch. In the “Network” field, enter “Delta Dental Premier”. If you visit a non-participating (Out-of-Network) dentist, you may be required to submit your own claim and pay for services at the time they are provided.
Cost to Use – There is no deductible for Preventive Services (Coverage A). For Basic services (Coverage B) and Major services (Coverage C) you will pay a one-time, Individual deductible of $100 or Family deductible of $300 with the Premium Plus plan. Under the Basic Plus plan, you will be responsible for a one-time, Individual deductible of $75 or Family deductible of $225.
The annual maximum for the Premier Plus plan is $2,000 per member. The annual maximum may be increased to as much as $4,000 per person with the Double-Up Max program.
The annual maximum for the Basic Plus plan is $1,000 per member. The annual maximum may be increased to as much as $2,000 per person with the Double-Up Max program.
See the attached Double-Up Max flyer for more information.
Premium Plus: After meeting the One-Time deductible, you will be responsible for 20% of the cost of in-network Basic services, 50% of Major services, and 100% of all services once you’ve reached your annual max of $2,000, unless you benefited from the Double-Up Max rollover provision. You would be responsible for orthodontia costs beyond $1,500 per member, per lifetime.
Basic Plus: After meeting the One-Time deductible, you will be responsible for 40% of the cost of in-network Basic services, 50% of Major services, and 100% of all services once you’ve reached your annual max of $1,000, unless you benefited from the Double-Up Max rollover provision. You would be responsible for orthodontia costs beyond $1,000 per member, per lifetime.
Cost to Own – What will your per paycheck deduction be? The amount that will be deducted from each paycheck is listed on the summary below.
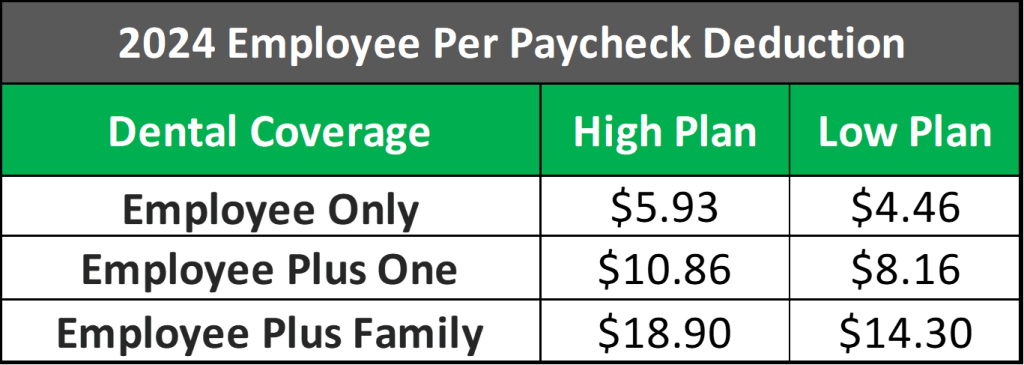
Enrolled employees pay premiums through payroll deductions, over 26 pay periods.
With Dental Insurance, it might be helpful to conduct a cost-benefit analysis for yourself and your family before enrolling. Once you’ve determined your annual cost to own the insurance, consider the following:
- How often do you and your family members receive preventive dental care?
- Do you expect to need major, non-cosmetic dental work in the coming year?
- Do you have a dentist you know and trust that is included in this plan’s network?
- Would making tax favorable elections/contributions to an FSA be a less expensive way for you to pay for dental care?
How do I enroll?
If you are electing coverage you’ll need to complete the Dental Enrollment form and return it to Human Resources.
Carrier Contact Information

Northeast Delta Dental: Dental Insurance
Customer Service: 800-832-5700
Website: www.nedelta.com
Plan Documents
Vision Benefits
Eligiblity
All full-time employees who work a minimum of 30 hours per week are eligible, first of the month following 30 days of employment.
Summary of Benefits and Coverages
Plan Overview
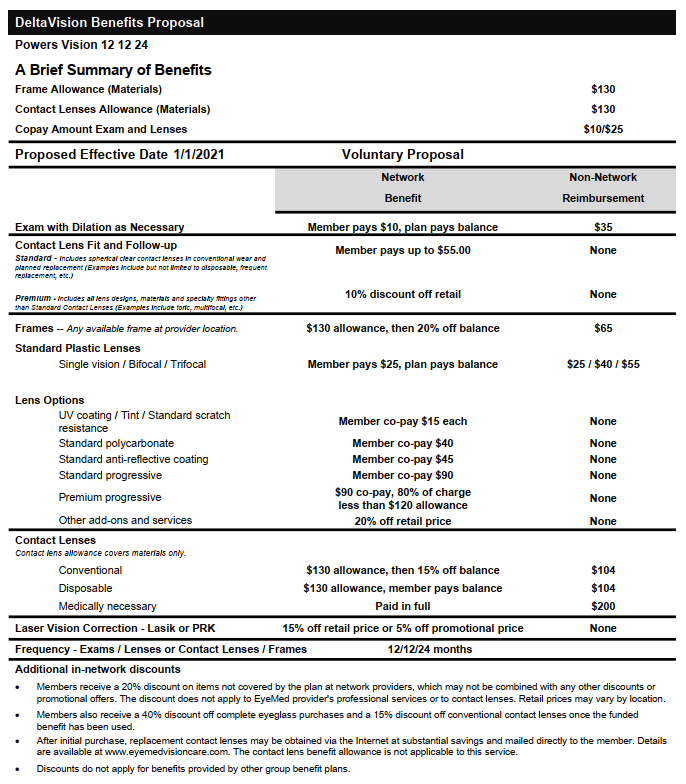
Powers offers a vision plan through Northeast Delta Dental and powered by EyeMed. If you are enrolled in the health insurance, some vision benefits are provided. The supplemental vision plan through Delta would offer additional, coordinated coverage.
Below, is a summary of features offered to eligible employees by Powers Guaranteed.
Network
To find and In-Network provider, go to: www.eyemedvisioncare.com
- Click “Find an Eye Doctor”
- Choose the Access Network
- Search by Location or Zip Code
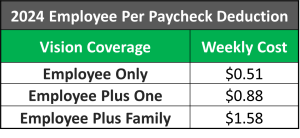
See your weekly payroll deduction below.
Vision Cost
Carrier Contact Information

Northeast Delta Dental and EyeMed: Dental Insurance
Customer Service: 800-832-5700
Website: www.eyemedvisioncare.com
Plan Documents
Group Life Insurance
Eligibility
All Active, Full-Time employees who work 30+ hours per week are eligible on the first of the month, following 30 days of employment.
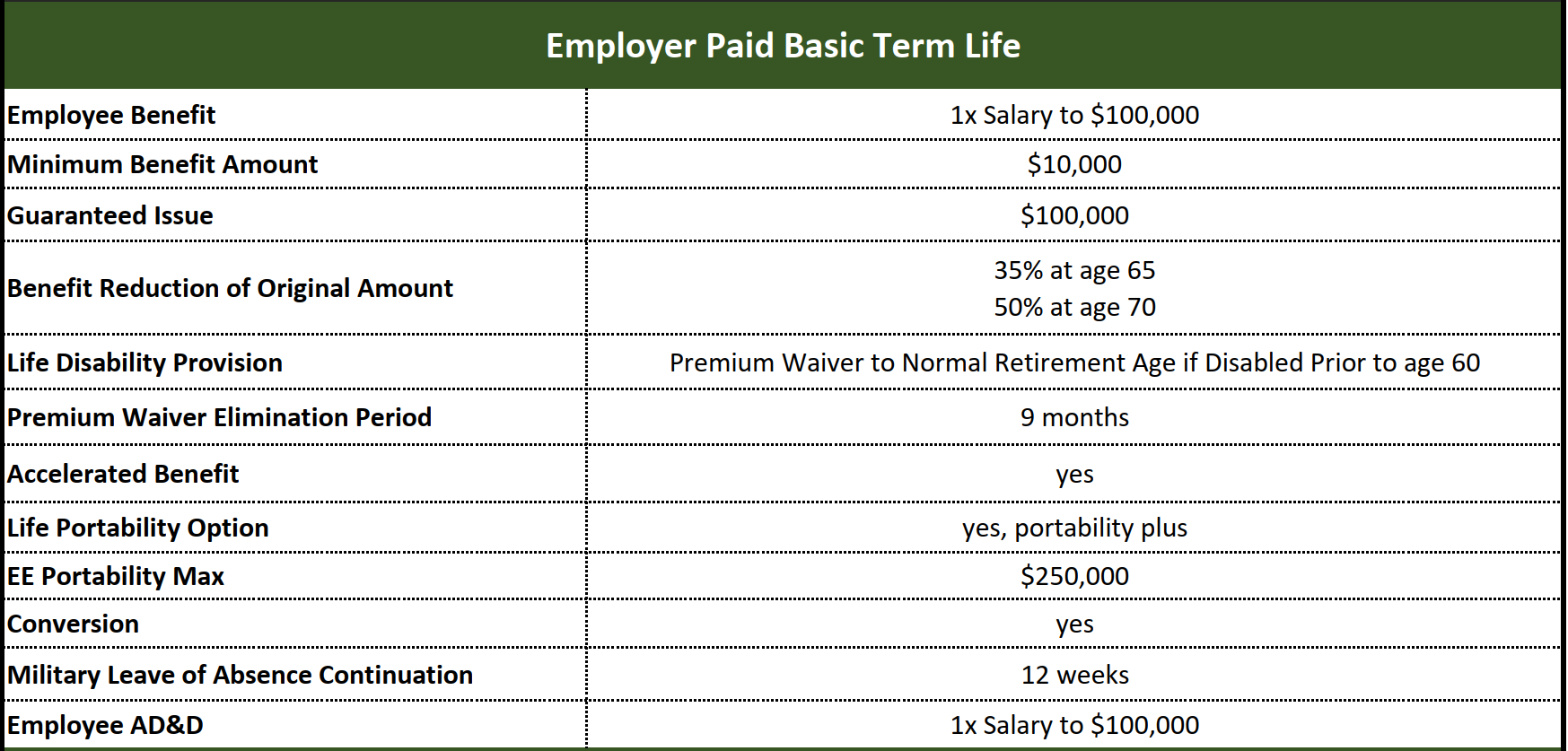
Summary of Group Basic Life and AD&D Benefits and Coverages
Insurance can play an important role in reducing financial stress when a family is faced with the pre-mature death or disability of a wage-earner.
To help employees during critical times of need, through UNUM, Powers provides employer paid Life Insurance to all full-time employees who work 30+ hours a week.
Basic Life insurance Benefits begin on the first of the month, following 30 days of employment with a benefit amount of 1X your salary up to $100,000.
Below is a table outlining the benefit coverage:
Voluntary Employee & Dependent Life Insurance
Families have unique circumstances and financial needs. Powers offers its Full-time employees who work 30+ hours per week, the opportunity to elect Voluntary Employee Life Insurance, Spouse Life Insurance and Child Life Insurance.
- Coverage is $5,000 – $500,000 depending on the covered member (employee, spouse or child)
- Employee – $500,000 maximum (Not exceed 3x earnings)
- Spouse – $100,000 maximum (coverage may not exceed 50% of employee amount)
- Employees will be required to submit a health application (EOI) if they elect coverage in excess of the guarantee issue amount
- Original Employee Supplemental Life benefit amount will reduce to 65% at age 65 and 50% at age 70
- Guaranteed issue amount (at initial eligibility period only) for Employee Supplemental Life is $100,000, and $25,000 for Spouse Life. All Child Life amounts are guaranteed issue.
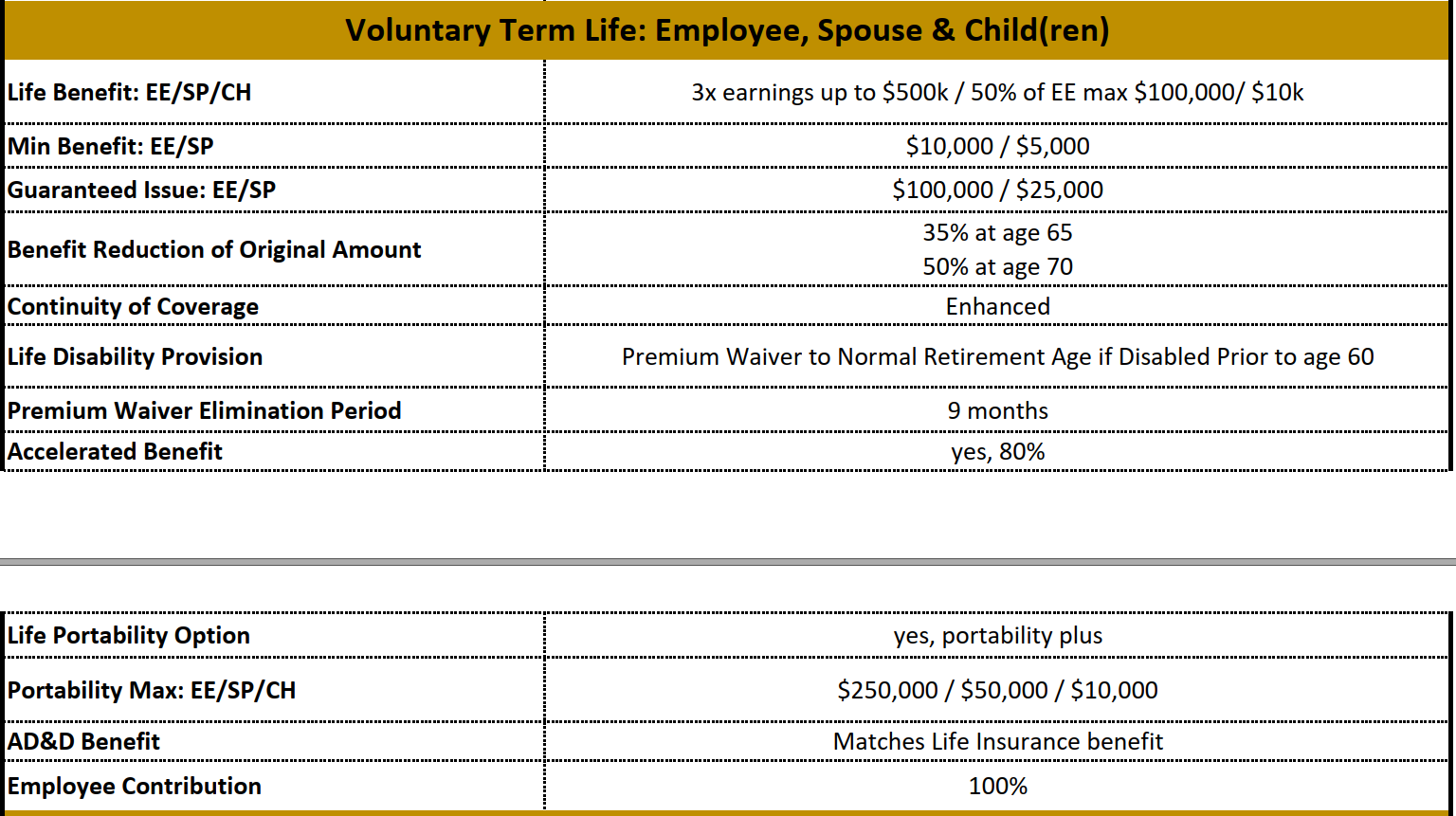
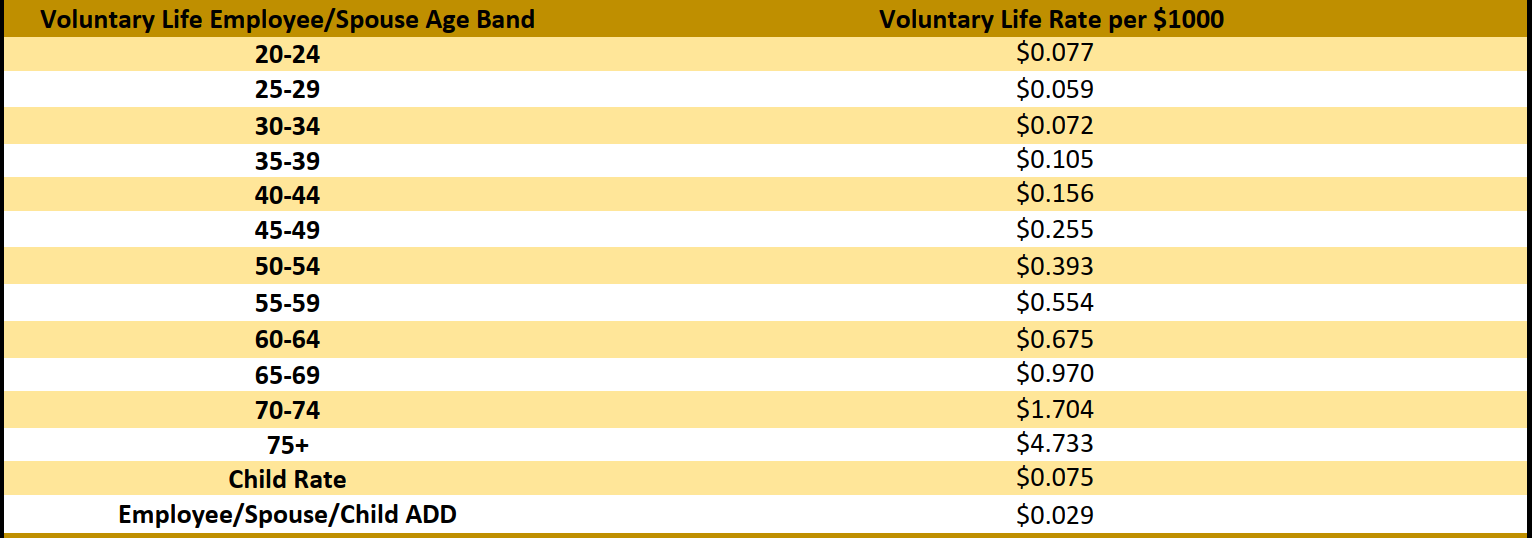
Below, are the monthly Voluntary Life Insurance rate calculations.
Carrier Contact Information

The Hartford: Life and AD&D
Customer Service: 800-523-2233
Website: www.thehartford.com
Contributions
Group Basic Life is 100% paid for by Powers.
Forms & Plan Documents
Long-Term & Short-Term Disability
Eligibility
All Full-Time employees who work 30 or more hours per week are eligible beginning on the first of the month, following 30 days of employment.
Summary of Benefits and Coverages
Most people don’t think about being disabled and unable to bring home their paycheck. Your financial obligations and living expenses don’t stop when you become disabled. Disability insurance can play an important role in reducing financial stress when facing the disability of a wage-earner.
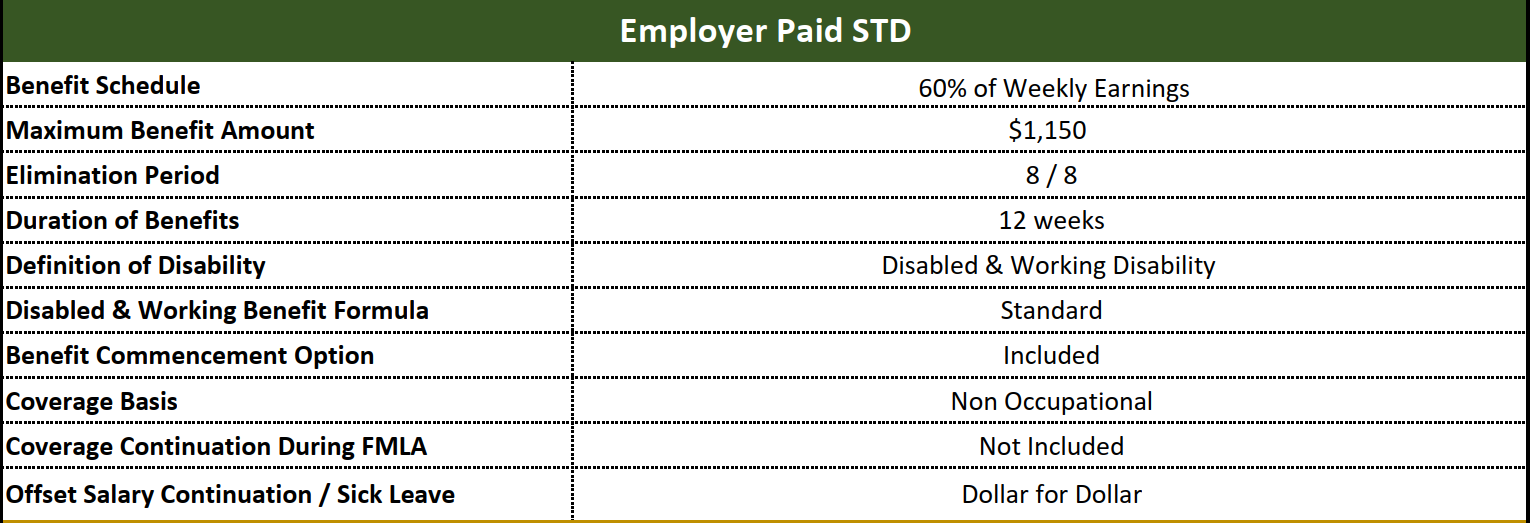
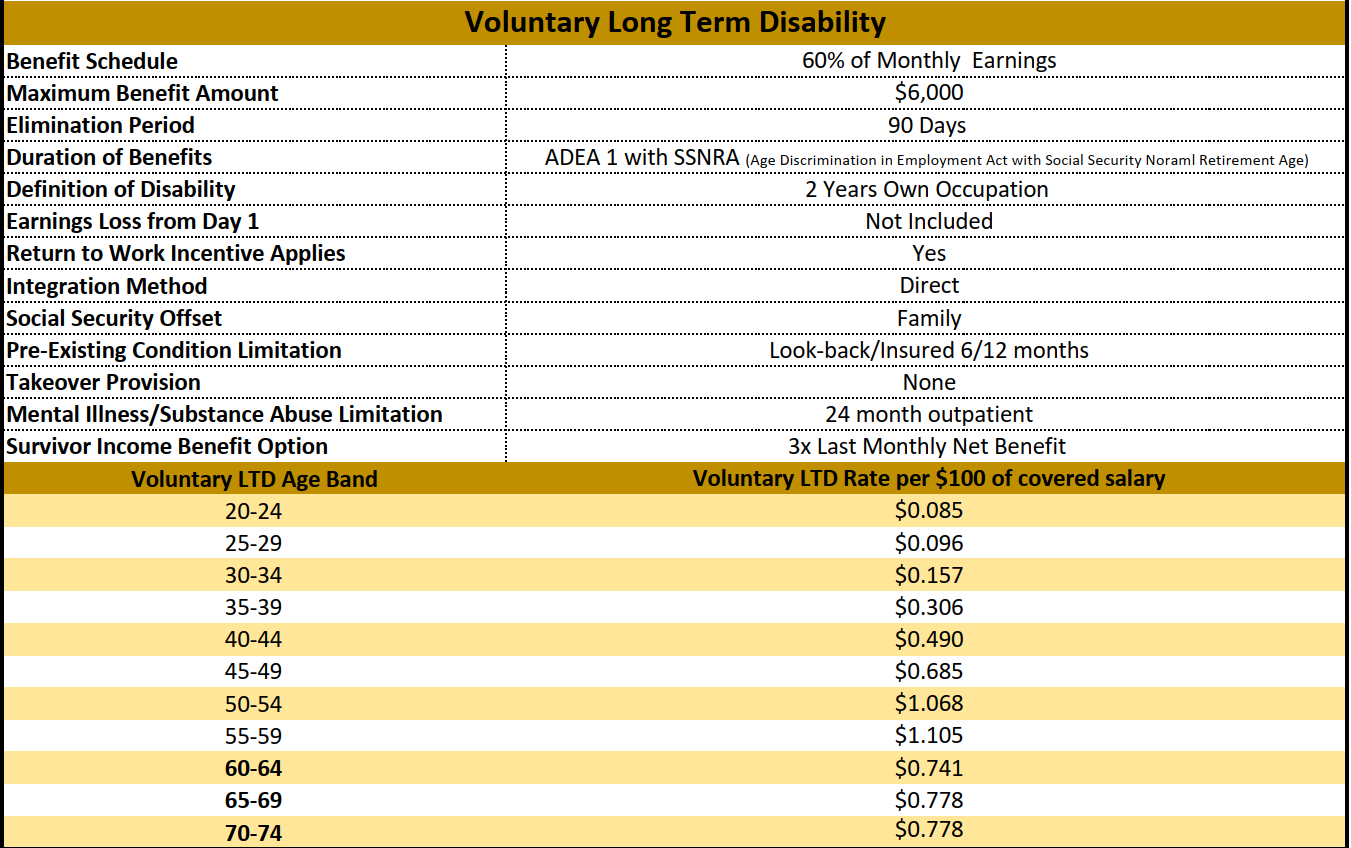
To help you during critical times of need, through The Hartford, Powers provides employer paid Short-Term Disability and Voluntary, employee paid, Long-Term Disability insurance to all full-time employees who work 30+ hours per week.
Below is a tables outlining the benefits & coverages:
Carrier Contact Information

The Hartford: Long-Term & Short-Term Disability Insurance
Customer Service: 800-523-2233
Website: www.thehartford.com
Forms & Plan Documents
401(k) Retirement Plan
IRA Details
Here at Powers, each eligible employee can make contributions into an Invesco IRA (Individual Retirement Account).
Why contribute to an IRA?
- Reduce your tax liability
- Close the gap between Social Security income and retirement expenses
- Compound your tax-deferred earnings
Key Points:
- You must be 21 Years of age or older to participate
- There is an annual maintenance fee of $25, paid by the employee
- Powers matches 100% of the first 3% of your earnings that you contribute
- Contributions to your IRA are made monthly
- Contributions are immediately vested at 100%
- Earnings are tax deferred.
For more information on how to enroll or to update your contributions, please contact Crystal Fish in Human Resources.

Invesco: IRA Retirement
Participant Services: 800-959-4246
Website: www.invesco.com
Additional Information
Employee Assistance Program
Employee Assistance Program (EAP) Details
Powers promotes the health of employees and their household members by offering immediate access to free, confidential counseling through Invest EAP, for a wide range of life issues. Invest EAP provides support for overall health, well-being and life management, the EAP can assist employees and their household members with issues such as everyday stress, grief & loss, legal questions, financial concerns and relationship issues at work or home. EAP benefits are 100% confidential and available to all employees and their household family members.
What is Invest EAP?
- Employee, Family, and Organizational Assistance Program
- 24/7/365 Free and confidential counseling, resources, and support for you
and your household members - Sometimes people just need a little support or free help to resolve
personal stress or problems - We are local to you and offer many of our services either in-person or via telehealth
Why do people call us?
▪ Counseling
▪ Resources
▪ Referrals
▪ Consultation
▪ Free legal referrals and financial advice
▪ Use us as a sounding board
▪ …And support for anything else that’s on your mind!

Invest EAP: Employee Assistance Program
Member Services: 866-660-9533
Website: www.investeap.org
Password: powers
Additional Information
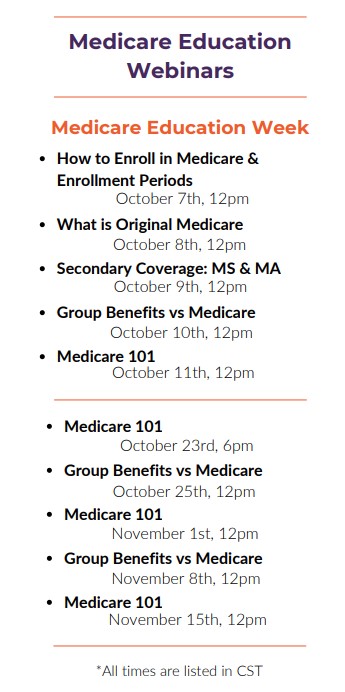
SmartConnect- Medicare Resource
The Richards Group has partnered with SmartConnect™, an exclusive, no-cost program created specifically to connect Medicare-eligible working adults to the world of Medicare benefits. Whether an employee plans to continue working or is transitioning to retirement, we tailor solutions designed around their needs. Our agents provide an unfiltered view of the entire range of options and prices available to the employee.
SmartConnect Contact Information
For more information or to get started, please click on the following link: https://gps.smartmatch.com/
Additional Information